...
The best way to deal with a deadly disease is to not get sick with it. But avoiding a disease can depend on how it’s spread, where you live or what you do for a living, and the possibility for a protective vaccine.
| Div | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||
|
Developing a Vaccine
| Div | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||
|
...
| Div | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||
|
Spencer had discovered that ticks were “a more efficient culture media than the guinea pig” if they went through incubation and feeding first.
- (Quote: "Rocky Mountain Spotted Fever: Experimental Studies on Tick Virus" Roscoe R. Spencer and Ralph R. Parker, Public Health Reports, Vol. 39, No. 48, November 28, 1924, pp. 3027-2040) 1.3 MB
| Div | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||
|
“The feasibility of human vaccination also naturally arises,” he wrote in his 1924 paper describing these studies. And he adds that he tried the vaccine on one human, with no ill effects. The human was himself.
- (Quote: "Rocky Mountain Spotted Fever: Experimental Studies on Tick Virus" Roscoe R. Spencer and Ralph R. Parker, Public Health Reports, Vol. 39, No. 48, November 28, 1924, pp. 3027-2040) 1.3 MB
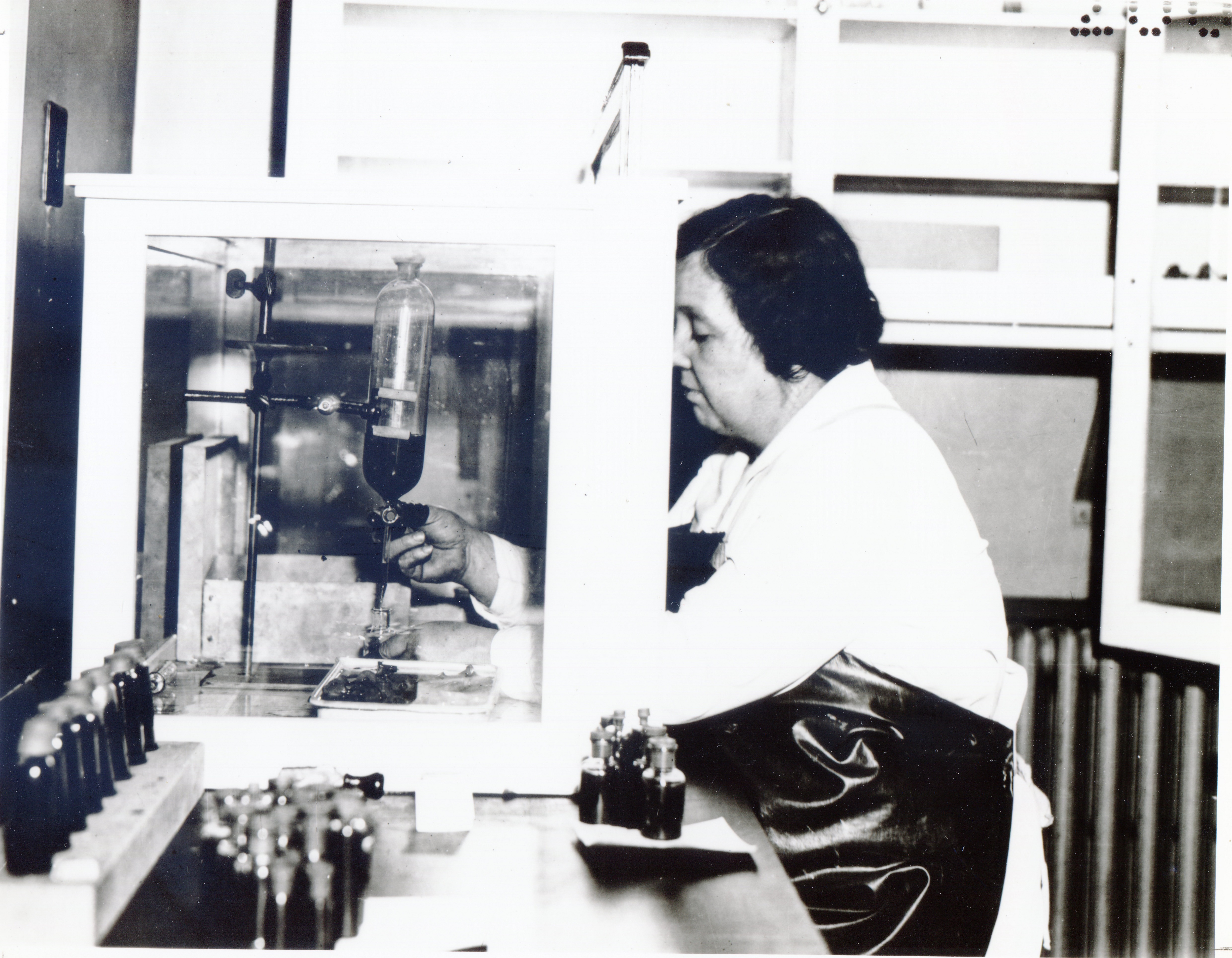
This bottle of Rocky Mountain spotted fever vaccine from the early 1940s represents much scientific work and practical experimentation. There were no strict research protocols for vaccine development and testing in the early 19th century. There was no oversight or approvals from the Food and Drug Administration. The Hygienic Laboratory (NIH’s precursor) had regulatory authority, testing commercial vaccines for safety and effectiveness. Spencer worked at the Hygienic Laboratory and was certainly familiar with the tests required to prove that a vaccine worked safely and at what dose it should be given, as well as the standards for producing a safe vaccine. He knew proving that his RMSF vaccine worked would take more than inoculating himself with it.
...
| Div | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||
|
...