hCG Research at NIH
For young researchers interested in reproductive hormone studies (reproductive endocrinology) in the late 1960s, the National Institutes of Health (NIH) was an ideal location. Two key researchers came to the NIH in1970 specifically to do research in this field. Judith Vaitukaitis and Glenn Braunstein, both medical residents in Boston (at different hospitals) in 1969, talked to their colleagues about where to pursue hormone research. Each heard the same message: go to Bethesda and talk to scientists Mortimer Lipsett and Griff Ross. Vaitukaitis arrived at NIH on a special postdoctoral fellowship and would become one of the first female senior investigators in her Institute. For Braunstein, NIH provided an opportunity to fulfill his military duty by signing up with the Public Health Service instead of going to Vietnam, and he came as a Clinical Associate.
Judith Vaitukaitis (JV): I came to [NIH to] stay for six weeks or six months, and I stayed almost six years. It was probably the most fun time of my life. It was the kind of scenario that, if I were independently wealthy, I would have done it for nothing.
JV: I think I may have been the first woman senior investigator [at NICHD]. But I was so used to it. In med school there were five or six women [in my class]. I can remember one of the guys walking up to me and saying, “You know, if you weren’t in this class, I’d be rated higher.” And I said, “Tough! Why don’t you work harder?” I’ll never forget that.
Glenn Braunstein (GB): I applied to go to the NIH to work with Griff Ross, but did not hear until the day before I was to sign my commission papers for the Army. The telegram said that I would be commissioned in the Public Health Service. This gave me the opportunity to fulfill my military obligation while working at the one place then on the cutting edge of hCG research.
The Reproduction Research Branch at NICHD, c. 1970.
Both young doctors arrived in Bethesda in 1970 and in the years they spent with the Reproductive Research Branch—first at the National Cancer Institute (NCI) and then at the National Institute for Child Health and Human Development (NICHD)—they found an active community for the study of reproductive endocrinology. Because of the newness of the field, they could practically publish a paper from every result.
JV: [The NIH] was one of the few places in the country where one could do reproductive endocrinology. It was a new field. And the thing was that no matter what we did, it was brand new, so everything was publishable.
JV: It was Building 10, 10B09. It was in a small laboratory, and for periods of months, there would be about 10 of us working in that space. I used to get over there about six o’clock in the morning and not leave till eleven o’clock at night. There were quite a few that worked long hours. The second or third year I was here, I think I published 28 papers in one year. They weren’t piddling kinds of things. I mean, there were so many things that one could do if you decided to think it through to understand what in the world’s going on. It was the way research should be.
Human Chorionic Gonadotropin (hCG) was a fascinating hormone to study in 1970, partly because not much was known about its behavior or makeup. Scientists did know that the human body secretes hCG only during pregnancy or during certain kinds of cancers. If they could find a way to precisely measure the hormone, they would have a reliable tumor marker, as well as a way to identify problems with a pregnancy. NCI’s Roy Hertz was studying a cancer called choriocarcinoma at the time. In this disease, patients exhibited tumors that secreted hCG. The clinicians wanted a way to test blood samples reliably for the presence of hCG so that they could track the tumor during treatment.
JV: We knew that the bioassay that was used for monitoring the amount of hormone they were measuring was very crude, very insensitive, but it was better than anything else we had at that time. So we needed another way of measuring the hCG in the presence of a finite amount of LH [luteinizing hormone].
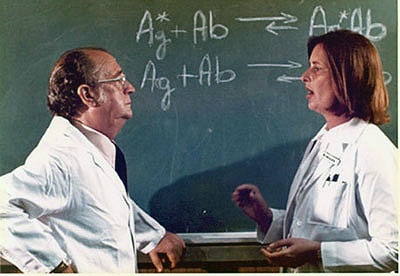
Griff Ross and Judith Vaitukaitis discuss their research, c. 1971.
JV: While we were doing this, we had no idea of the impact on early pregnancy detection, abnormal pregnancy detection. In ectopic pregnancy, the levels of hCG usually start falling and they don’t rise as high as they do within a normal pregnancy.
However, measuring precise levels of hCG is exactly what the bioassays of the mid-twentieth century and the immunoassays of the 1960s could not do. The best test they had in 1970 was an immunoassay that could measure hCG but could not distinguish between hCG and luteinizing hormone (LH), another of the human gonadotropins that shares its biological characteristics.
GB: Griff and I spoke. “Wouldn’t it be great to develop a new assay for hCG.” At that time Judy Vaitukaitis was immunizing rabbits with subunits of hCG and harvesting antibodies.
Vaitukaitis was working at separating the subunits of hCG and determining their biological function and characteristics. In 1970 and 1971 she worked on generating an antibody that would be specific to the beta-subunit of hCG and that could therefore be used in a radioimmunoassay—so called because the process used radioactive labels in the immunoassay—and would not cross-react with other hormones in the body. In 1972, she found it. The first rabbit to produce the antibody was called “SB6” and became the baseline for future experiments.
JV: We were looking at structure-function studies of human chorionic gonadotropin. Was there biologic activity in the isolated subunit? What was it about the molecule that was responsible for the unique immunologic and biologic activity? Then we realized that the biologic effect of the hormone resided in the beta unit of hCG. So in doing these structure-function studies to understand where the immunologic and biologic specificity resided, it became obvious that you could really take advantage of the relative specificity of the antiserum.
JV: It was critical for [NICHD’s] John Robbins to be involved with this because he had the immunology background. Actually, we tried two doses of immunogen [to make the antibody], 10 and 50 micrograms, and so the animal that had the first dose of 50 micrograms of immunogen was labeled SB6, since it was the sixth rabbit. There were five rabbits immunized with 10 micrograms, and we were told they would never make antibody at 10. I said, “Let’s see.” We went down subsequently to 2 and showed it would respond at that, too. So the first animal that was immunized with 50 micrograms, SB6, became the classic antiserum that had the best relative specificity that was used for years, and we provided it all over the place.
At NIH, scientists at intramural institutes in Bethesda have the opportunity both to work at the laboratory bench and follow patients at the Clinical Center. Though the Reproductive Research Branch had moved to NICHD, the scientists collaborated with cancer researchers at NCI. Vaitukaitis and her colleagues examined patients with choriocarcinoma, a type of cancer in which patients showed elevated levels of hCG. While simultaneously working on purifying and developing tests for identifying hCG in human serum, they could study both current Clinical Center patients and blood samples previously collected by the NCI and frozen for research.
JV: In screening some of these patients, we routinely took blood and measured hCG in them. We started turning up hCG levels in some of these patients. This was brand-new territory. But here we were working in a laboratory—it really underscores why you need physicians to be involved with clinical research. If you can make the diagnosis, you had a way of treating the disease.
Working on an experiment, NICHD, c. 1971.
GB: So we went to the freezer. Griff Ross had serial samples from women with choriocarcinoma and we put those samples into the assay. Some of the women who were supposed to be cured actually still had hCG. We started to look at other types of cancers, too. Tom Waldmann at NCI also had a freezer full of blood samples from cancer patients, both single and serial samples. We put the samples through the assay, and found that 18% of the nontrophoblastic tumors showed levels of hCG. This was news: hCG was a tumor marker for non-trophoblastic tumors as well as trophoblastic tumors.
Research at NIH, as elsewhere, is a collaborative experience. Griff Ross’ group needed some basic research tools to do their studies, including, among other things, purified hormone and urine from post-menopausal women. These substances would be used for experiments as the scientists learned more about hormones and the human body. The group used hCG purified by NICHD grantee Robert Canfield, known as the CR preparation of hCG, for “Canfield-Ross.” For other research supplies, they turned to some unusual sources.
JV: Canfield’s laboratory was isolating the human chorionic gonadotropin from the pregnancy urine, and he had isolated it and broken it down to two subunits. That was back in the days where you had to do things by hand, and so the throughput was very slow and tedious.
JV: We were doing studies on follicle-stimulating hormone [FSH]. It was like hCG but it has a different biologic effect. We wanted to study the biologic effect of FSH, so we contacted a retirement home for nuns and arranged with the nuns to collect their urine and put it in these big plastic containers. [We would] go over there once a month with somebody who was strong enough to lift these bottles. I would say probably each plastic container held probably about 15 gallons of urine. We would take it back and then process it to isolate the FSH from it, [and] then use that to study what the effect of sialic acid was on hormone action. It was unbelievable, but we got a lot of stuff done with that. I would never want to do it again!
In 1972, Vaitukaitis, Braunstein, and Ross were ready to publish their major paper on hCG research, in which they described their methodology for using antibodies to the beta subunit of hCG in a radioimmunoassay to identify and measure hCG in the presence of LH. Before publishing, they met with the NIH lawyers to discuss patenting their process. Surely none in the room that day could have predicted the multi-million dollar business that the home pregnancy test would become within the next few decades. However, the test’s usefulness as an accurate tumor marker alone might have justified the patent, since by then the team had already used the test on Clinical Center patients and proved its reliability. But NIH declined to patent the test. Since the work was done using public funds, went the argument, the results should go immediately into the public domain, with no royalties for either the government or the scientists. This policy has since been changed. NIH now submits patents listing the scientists as co-inventors, and the scientists can receive limited royalties from their discoveries. But the millionaire’s life was not to be for the NICHD researchers.
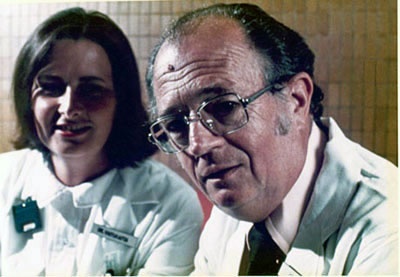
Judith Vaitukaitis and Griff Ross ca. 1971
JV: One of our concerns was that we [had] developed this assay and we wanted to protect the public from getting gouged with being charged for these tests, because we knew it would be picked up by the commercial outfits. But the legal counsel [of NIH] would not at that time allow patenting.
GB: We knew this would be a fantastic pregnancy test. We went to the government lawyers and said, “This is a technique that is going to be extraordinarily useful. Why not have NIH profit from it?” But since it was developed with public funds, the lawyers said no.
In the 1970s, the researchers went on to other subjects. Vaitukaitis returned to Boston to spend a decade at the Boston University School of Medicine before returning to the NIH in 1986 to work with the division that would become the National Center for Research Resources (NCRR). She has served as Director of NCRR since 1993. Glenn Braunstein went to California, where he continues research on hCG and other reproductive hormones at Cedar-Sinai Medical Institute in Los Angeles. In his long and illustrious career at NIH, Griff Ross would attain the posts of chief of the Endocrinology and Reproduction Research Branch, clinical director of NICHD, scientific director of NICHD, and associate director of the Clinical Center.
In 2003, as NICHD celebrated its fortieth anniversary, Institute Director Dr. Duane Alexander singled out the pregnancy test research as some of the most seminal work done by the Institute over its four decades. Judith Vaitukaitis was inducted into the NICHD Hall of Honor “for discovery of the beta subunit of human chorionic gonadotropin and identifying it as the earliest marker of pregnancy, leading to its development as the standard pregnancy test and as a monitor for response to cancer treatment.”
Note: Quotations labeled “JV” are from an interview with Judith Vaitukaitis, August 18, 2003. Quotations labeled “GB” are from a telephone conversation with Glenn Braunstein, October 3, 2003.